Corresponding author for proof
Alessandro Varini, MD
Casa di Cura Salus, Trieste, Italy
Via Bonaparte 4, 34123 Trieste, Italy
varini.alessandro@gmail.com
Tel +390403171111
Coauthors addresses:
Nicola Bianco, MD, PhD
Casa di Cura Santa Rita, Atripalda (Avellino), Italy
Via Appia snc, 83042 Atripalda (Avellino), Italy
dottnicolabianco@gmail.com
Tel +390825629111
Cristina Diana, MD
Casa di Cura Santa Maria, Bolzano, Italy
Via Claudia dè Medici 2, 39100 Bolzano, Italy
cristina.diana@alice.it
Tel +390471310600
The authors have nothing to disclose.
Keywords: rhinoplasty, nose tip, tip surgery, tip graft, tip projection, tip shape.
Abstract
Nasal tip projection is recognized as critical in nasal aesthetics. A patient’s happiness and surgical success are often determined by the quality of tip surgery. Various techniques have been described to achieve adequate tip projection. In this article we report our experience with the onlay tip graft, modified from the original graft conceived by Peck. Details of the technique and discussion and analysis of the literature are presented.
Introduction
Tip surgery is recognized as the most challenging part of cosmetic rhinoplasty. “The tip makes the nose” (1). One essential aspect in analysis and planning is nasal tip projection. After dorsal reduction the nasal tip must be adequately projected. In the majority of rhinoplasties a maintenance or an increase of tip projection is required.
One more critical factor in rhinoplasty is tip contour and shape, which is determined by the shape of the domes and the relationship with the lateral and the intermediate-medial crura. The skin soft tissue envelope and ligaments interact with the underlying cartilaginous framework. Thickness of the soft tissue envelope affects the surgical result and is highly variable. Thorough understanding of the anatomy and tip support mechanisms is paramount (2).
Many methods have been proposed to assess tip projection and many techniques have been described with the purpose of controlling and modifying projection.
Tip surgery has evolved from excisional to suture and grafting techniques.
The choice of the technique depends on surgical and patient factors, such as size, strength and shape of cartilages and quality and thickness of the soft tissue envelope.
Conventional surgical techniques based on sutures can be enough to modify tip projection and to achieve better tip definition. In some instances more volume and structure can be obtained by using grafts, to project the tip to the desired level.
The tip onlay graft was originally described and popularized by Peck in 1983 (3). The Peck tip graft can be useful in increasing tip projection and definition. The main indication is loss of tip projection but the graft can also be used to provide contour and shape and to modify tip rotation.
Technique
Tip grafts have the advantage of providing tip projection and definition.
Tip projection can be assessed as excessive, adequate or inadequate. Each routine incision in rhinoseptoplasty usually alters the tip support mechanisms and, as a consequence, reduces tip projection. Conventional transfixion incision combined with intercartilaginous incisions result in decreased projection.
Normal projection can be difficult to judge. In some patient tip underprojection is not easily identified preoperatively. The perception of nasal projection is strongly influenced by the dorsal height. Signs of underprojected tip can be short columella and/or lobule, acute nasolabial angle, maxillary retrusion and small, weak alar cartilages (4).
If the anterior septal angle is visible and higher than the nasal tip, a tip graft can be indicated.
The height of the graft, and the resulting bulk, affects the depth of the supratip break.
The tip onlay graft can increase tip rotation. Tip rotation is most commonly assessed on the profile view of the nose. Historically, there have been two methods of measuring nasal tip rotation: the nasolabial angle (NLA) and the nostril axis (NA). Rotation, and nasal length, can also be measured by three different axes, formed by a line between nasion and 1) subnasale, 2) infratip break point, 3) pronasale. The length of the nose, formed by the distance between the nasion and the tip defining point (pronasale), may be adjusted by cranial or caudal placement of this graft.
We have been using the tip onlay graft for many years. Our indication in primary cases is the underprojected tip or the tip with normal projection when, after incisions and other maneuvers, is at risk of losing projection. One more indication is the underrotated tip and excessive length. Poor tip definition can be ameliorated by using this graft. Thick soft tissue envelope usually benefits from tip augmentation by grafting. In secondary rhinoplasty, violation or overresection of the domes is also an indication for tip onlay graft.
The procedure is characterized by a stepwise approach, since tip projection can be accomplished by using different techniques in a graduated fashion (5). The use of the tip onlay graft is planned during preoperatory analysis.
In most cases, authors an endonasal approach. The planned position is rarely marked onto the skin.
Before placing the graft, structural adjustment of the supporting structures must be completed. Alar cartilages are delivered through marginal and intercartilaginous incisions. The first surgical step is to ensure adequate tip support and to correct the intermediate-medial crura length and symmetry. Interdomal and transdomal sutures are positioned and a columellar strut is used when more support is needed. If the domes are uneven, a cephalic dome equalization suture can align them (6). Sutures of the intermediate crura and lateral crural steal, septo-columellar sutures or anchor sutures between caudal septum and medial crura can affect projection and must be completed before positioning the tip onlay graft.
The onlay tip graft is placed transversally over the domes. This is the difference compared with the shield Sheen graft (7), which is positioned over the intermediate crura and is mainly indicated for extending short intermediate crura. According to Peck (3), the position of the graft “although it usually corresponds to a position horizontally over the domes, it can understandably be either slightly cephalad or caudad to the domes”. Cranial or caudal positioning invariably influences nasal length and rotation.
The graft is typically carved from septal cartilage even though any cartilage may be used, such as the auricular one from concha cymba and cavum. Thickness of the graft depends on the thickness and condition of the skin. Thick-skinned patients need thicker graft to resist the pressure of the soft tissue envelope. Sculpture of the graft must be accurate. In thin-skinned patients, thick septal cartilage often require scoring, the edges of the graft must be beveled and the corners rounded. Cartilage obtained from the hump resembles the shape of the two domes.
The shape of the graft can be oval, rectangular or triangular. Our choice is to use an isosceles trapezoid shape with the base directed caudally in order to create new tip defining points. The base or caudal border of the graft sets the width of the tip, i.e. the interdomal distance. A notch can be created along the base to mimic the tip highlights. The superior surface can be shaped to simulate the natural shape of the two domes. The graft may be single, double or multilayered.
The graft is commonly sutured (4/0 or 5/0 PDS or monocryl) laterally to the lateral crus on both sides, to prevent slippage or shifting and to create a soft curvature, with a gentle transition from the new dome unit towards the lateral crura.
The risk of visibility of the graft can be addressed by covering it with cartilage or fascia. The cephalic aspect of the lateral crura has shown to be very useful because of its elasticity, thinness and pliability and it may be used especially to camouflage the graft underneath. Crushed cartilage or diced cartilage may be added and placed superficially. A combination of solid and crushed cartilage can reduce the risk of the graft showing. The pericondrium/periosteum of the hump, soft tissue and scar tissue are also useful. When the graft is tenting through the skin, it should be removed and reshaped to avoid visibility.
The alar cartilages are preserved intact for support. If more tip stability and support is requested, the onlay tip graft may be combined with a columellar strut (similar to the umbrella technique (3). The columellar strut is also indicated when the patient has a short columella, a narrow nasolabial angle and a retracted subnasale. Tip projection can be obtained by advancing the medial crura onto the strut. The shield Sheen graft can be added, and sutured to the Peck graft, when tip derotation, increase of the intermediate crura length and better definition of the lobule are required. The main indication of the Sheen graft is infratip lobule deficiency. In this case the Peck graft can also act as a buttress behind, limiting the cephalic rotation of the Sheen graft (Fig. 9).
Discussion
For successful tip surgery, according to Costantian (8), there are two critical anatomical characteristics to be analyzed in rhinoplasty candidates, and one is if the tip is adequately projecting. In 1995, Peck et al. stated that the most frequent indication for secondary rhinoplasty is the inadequately projecting nasal tip and therefore he used the onlay graft in approximately 85% of all primary cases (9).
Various techniques have been proposed in the literature.
The suture technique can be effective in maintaining or gaining projection. Lateral crural steal and tongue in groove are good example of valuable techniques (10,11). The tip onlay graft should be used selectively, when tip sutures cannot accomplish good results (12).
The tip onlay graft was conceived by Peck (3) with the aim of providing projection to the nasal tip. In his article he reported the experience of 152 patients over a 5-year period. Peck stated that, as a lesson from 20 years of experience, the integrity of the domes must never be violated. The author cited the tip button graft (13), the columellar strut graft (14,15) and the Sheen graft, reporting the shortcomings of these techniques such as visibility and skin tenting. Peck originally described a graft obtained from auricular conchal cartilage, positioned through a rim incision in a pocket overlying the domes, whose size was made just large enough to accommodate a graft of average dimension of 4 x 9 mm. If the pocket was too large, the graft could be sutured using a pull-out suture. The natural convexity of conchal cartilage simulates the curvature of the tip. Other sources he used were the cephalic part of lower lateral cartilages, cartilaginous hump and septal cartilage, which often required scoring. If more projection was desired, he used a double-layered graft or he combined the horizontal onlay graft with a vertical strut placed between the medial crura (umbrella technique). The umbrella graft was the subject of a subsequent article (16), where the authors reported the use of this graft in 22 percent of 1252 cases in a 10-year period, most secondary, requiring tip projection and support. Indications for the umbrella graft included drooping nasal tip, parrot beak deformity, wide and flat nose or overshortened nose, cleft lip nasal deformity and the thick sebaceous tip. Revision rate was 5 percent, and the commonest complication was graft show.
In 1972, Sheen introduced his shield graft as a technique for achieving more tip projection (17).
In 1993, Sheen analyzed his own personal experience in using nasal tip grafts over the previous 20 years (18). The graft was originally used for secondary rhinoplasty and for primary patients with inadequate projection. The graft pocket was created through a right-side marginal incision, extending the dissection posteriorly not beyond the columellar-lobular junction. Infection and displacement apart, one problem was a potential flatness of the caudal surface of the lobule, later solved by adding a small piece of crushed cartilage. In the next period, Sheen expanded the indication of the graft for tip distortion, and he used the graft in all thick-skinned ethnic patients. Ethmoid and vomer bone graft were abandoned. Multiple grafts became routine, due to the correlation with tip contour, but overaugmentation became a risk. In the last analyzed period, Sheen added more applications, for correcting malpositioned and convex lateral crura, variations and disproportions of middle and medial crura.
In 1998, Adham et al. suggested a modified cartilage disc tip graft, consisting of two stacks of cartilage disks with a piece of the cephalic part of the alar cartilage on top, fixed to the (old) domes in three points (19). The advantages reported were maintenance of independence of each tip-defining point.
In 1999, Porter at al. described the contoured auricular projection graft in selected patients for achieving satisfactory tip projection and natural rounded tip in patients with blunted tips, such as Asians, African Americans and selected patients with revision rhinoplasty (20). The graft was placed endonasally in a precise pocket or sutured by an external approach.
The original rectangular shape of the graft was modified by Guyuron (21) into a “B”, resulting in two-point definition.
Nasal tip silicone sizers were developed and used by Gruber (22) to observe the best width and the best location before securing the graft. Sizers helped select the size and shape of the graft and reduced the risk of wasting donor material.
In 2005, Pastorek et al. proposed an evolution of the Sheen tip graft for the underprojected tip, the extended columellar strut-tip graft, which combined the countering shape of the tip graft with the strength of the columellar strut into a stable unit (23). The graft had the shape of a long isosceles triangle, 2.5 cm in length and 8-12 mm in width, flexible and curved. The graft was not sutured and it was inserted endonasally into the precrural space through marginal incision, after wide undermining, as the final maneuver. Tight suture closure of the marginal incision was able to control graft shifting.
In 2007, Guyuron et al. suggested an additional modification of the classic rectangular Peck graft, since it does not resemble the anatomy of two separated domes and the resulting light reflections (24). The reported drawbacks of the tip grafts, related to the technique of sculpting, prompted the authors to design a new instrument, the tip graft punch. The biorbicular superior and anterior part of the graft is sutured to the domes and the inferior and posterior columellar segment is fixed to the intermediate crura.
In 2009, Daniel described the tip refinement graft (TRG), made from excised lateral crura with a variable shape, domal, shield, diamond, folded or combination (25). Open tip sutures showed limits in thick-skinned patients. These grafts were positioned to gain more definition and to increase projection. The domal TRG were small pieces, 8×4 mm, placed over the domes and designed to accentuate tip definition and to create a subtle set-off relative to the dorsal line. A TRG was used in 59% of 100 consecutive cases.
Cartilage grafting has become an essential step in tip reconstruction in revision surgery. One common problem in secondary rhinoplasty is the loss of tip projection and contour caused by overresection of the alar cartilages (18). Kridel and Soliemanzadeh (4) analyzed indications and techniques for tip grafts in revision rhinoplasty. The pollybeak deformity is one of the commonest causes of revision rhinoplasty and the commonest contributing factor is the underprojected tip with poor support (26,27).
Conclusion
Closed or external approaches offer similar potential for positioning. Positioning and stabilization are usually easier using an open approach. In the closed approach, the Peck graft can be placed in a floating fashion and inserted in a precise pocket overlying the domes, with or without a “U” transcutaneous suture (28) or secured directly to the domes using sutures.
As for other grafts, the tip graft should be used more cautiously in thin-skinned patients. Tip bifidity, dome irregularities and asymmetries can be corrected with this graft.
Increase in tip definition in thick-skinned patients can be mainly achieved by grafting. The combination of thick skin and excess fibrofatty tissue with weak lower lateral cartilages is an indication for graft augmentation to provide better definition and refinement.
Despite improvements in techniques for cartilage grafting, some problems might still remain such as malposition, displacement, cartilage warping, visibility, soft tissue envelope deformation and atrophy, graft extrusion, infection and resorption and long-term integrity of the graft.
Even if some grafts can lose strength and partially absorb over time, resorption of the tip graft was not considered by Peck to be of concern. Graft slippage or shifting can be avoided by precise suture fixation of the graft, which is possible with both, open or closed approaches. Graft visibility is not an issue in thick-skinned patients. Instead, in thin-skinned patients the graft should always be covered by fascia or percondrium or thinned/crushed/diced cartilage.
The potential of the tip onlay graft for increased control over support, projection and contour has led to satisfactory and predictable results in our patients.
Clinical cases

Fig. 1. (left) Preoperative right profile of a 20-year-old female and (right) postoperative result 1 year later. A tip onlay graft was used to give tip projection and rotation and to shorten the profile line.

Fig. 2. Preoperative (left) and postoperative (right) base views of the same patient of fig. 1, showing the improvement in tip shape by using the graft for correcting short intermediate crura.

Fig 3. The same patient of fig. 1 and 2, preoperative (left) and postoperative (right) left profile views, showing the improvement in the supratip break.


Fig. 4. Preoperative (left) and 1-year postoperative (right) profile views of a 26-year-old male patient. He was at risk of developing a pollybeak after the operation due to the high anterior septal angle. After cephalic trimming of lateral crura, interdomal and domal equalization sutures were used to stabilize the tip supporting anatomic structures. The tip onlay graft was used to achieve adequate tip projection and rotation.
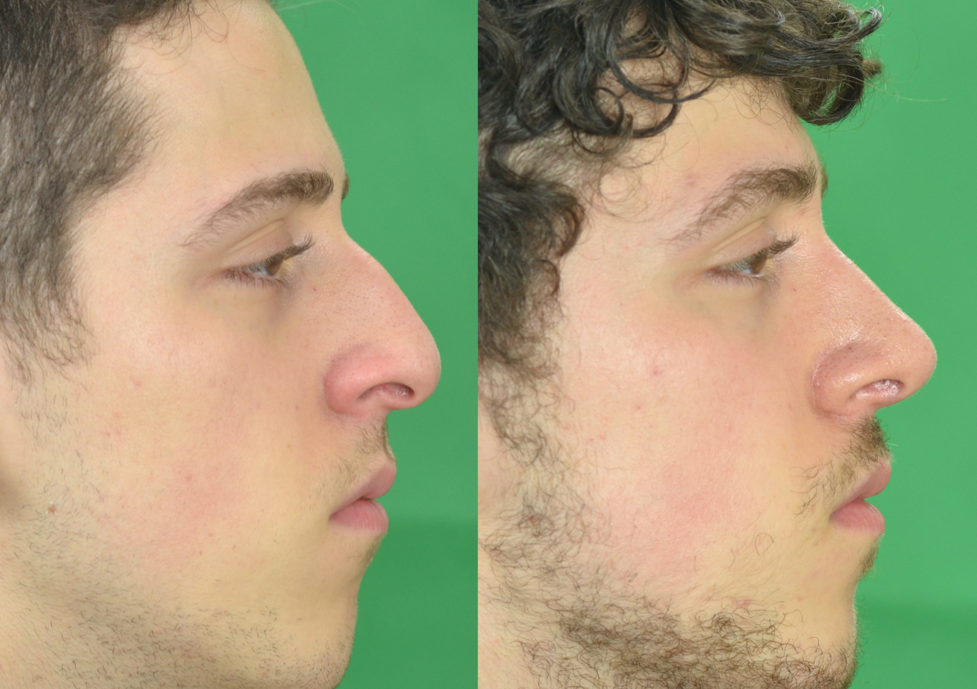



Fig. 5. Preoperative (left) and one year postoperative (right) views of a 22-year-old male patient with a modified onlay tip graft to increase tip definition and to improve tip projection. The graft was placed after the interdomal and transdomal sutures to narrow the interdomal distance and domal angle.





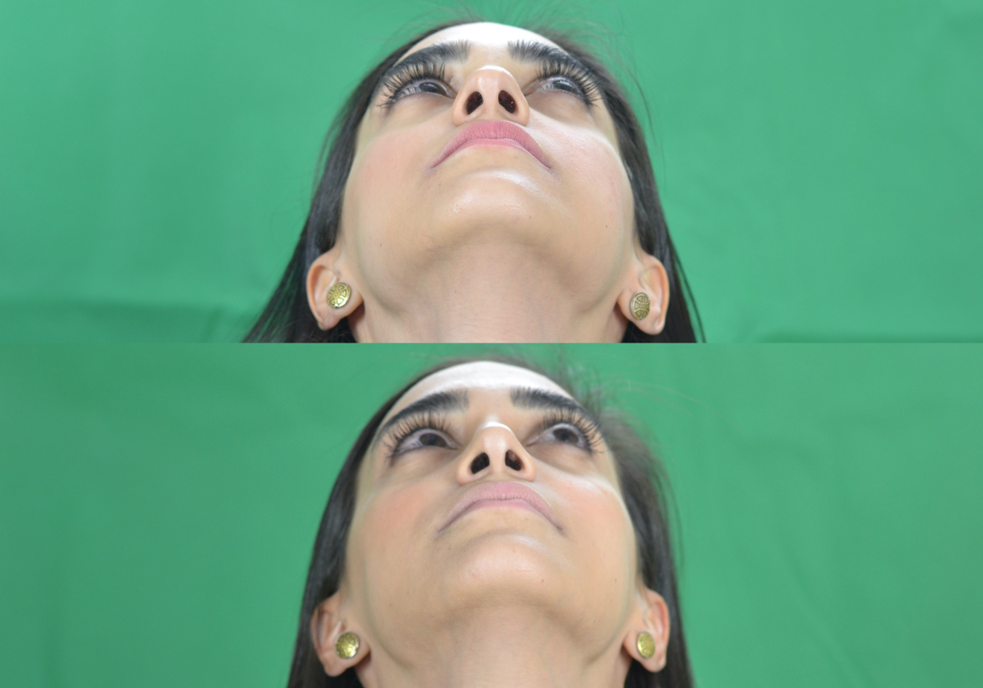
Fig. 6. Standard preoperative and 1 year postoperative rhinoplasty views of a 19-year-old female patient who underwent a closed approach with onlay tip Peck graft.



Fig. 7. Standard preoperative and 1 year postoperative rhinoplasty views of a 22-year-old female patient who underwent an open approach with onlay tip Peck graft.
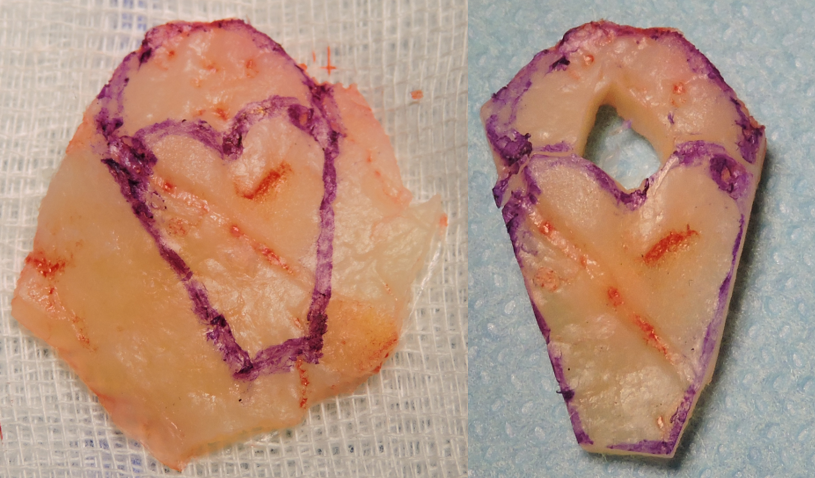
Fig. 8. An example of a combination of Sheen shield graft and Peck tip onlay graft harvested from septal cartilage (presented at the 2016 EAFPS congress London).
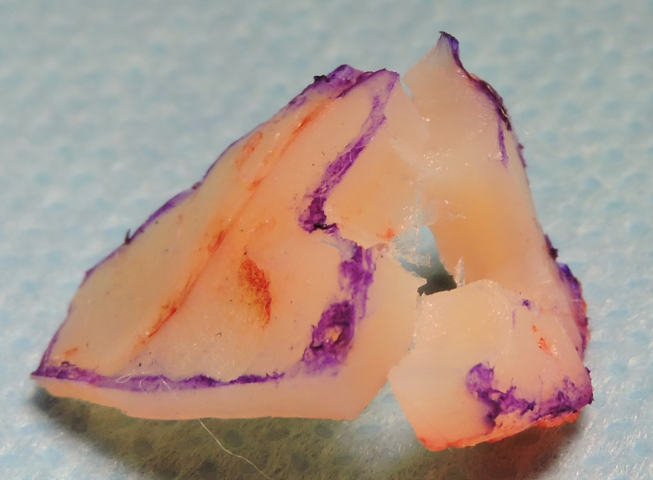
Fig. 9. The tip onlay graft can act as a buttress cranially, limiting the rotation of the shield graft (presented at the 2016 EAFPS congress London).

Fig. 10. Intraoperative view of a patient with the tip onlay graft carved from the cephalic trim (29), secured on a stable basis made of medial crura and columellar strut.

Fig. 11. Same patient of Fig. 10. The trapezoidal shape of the graft reproduces the typical divergence of the domes.

Fig. 12. Same patient of Fig. 10 and 11. The graft is sutured on to the domes with 4-0 PDS.
References
- Goldman IB. New technique for corrective surgery of nasal tip. AMA Arch Otolaryngol. 1953;58(2):183-187
- Petroff MA, McCollough EG, Hom D, et al. Nasal tip projection. Quantitative changes following rhinoplasty. Arch Otolaryngol Head Neck Surg. 1991;117(7):783–788.
- Peck GC. The onlay graft for nasal tip projection. Plast Reconstr Surg 1983;71(1):27-39
- Kridel RWH, Soliemanzadeh P. Tip grafts in revision rhinoplasty. Facial Plast Surg Clin North Am 2006;14(4):331-41
- Hackney FL, Gunter JP. Increasing and decreasing tip projection in rhinoplasty. Op Tech Plast Reconstr Surg 2000;7(4):168-74
- Daniel RK. Rhinoplasty: a simplified, three-stitch, open tip suture technique. Part I: primary rhinoplasty. Plast Reconstr Surg 1999;103(5):1491-502
- Sheen JH. Achieving more nasal tip projection by the use of a small autogenous vomer or septal cartilage graft. Plast Reconstr Surg 1975;56:35-40
- Costantian MB. The Two Essential Elements for Planning Tip Surgery in Primary and Secondary Rhinoplasty: Observations Based on Review of 100 Consecutive Patients. Plast Reconstr Surg 2004;114(6):1571-81
- Peck GC et al. Inadequate tip projection: the most frequent problem in secondary rhinoplasty. Op Tech Plast Reconstr Surg 1995;2(1):49-54
- Kridel RWH, Konior RJ, Shumrick K, et al. Advances in nasal tip surgery: The lateral crural steal. Arch Otolaryngol Head Neck Surg 1989;115:1206-1212
- Kridel RWH, Scott BA, Foda HMT. The Tongue-in-Groove Technique in Septorhinoplasty. A 10-Year Experience. Arch Facial Plast Surg. 1999;1:246-256
- Tebbets JB. Shaping and positioning the nasal tip without structural disruption: a new, systematic approach. Plast Reconstr Surg 1994;94(1):61–77.
- Fomon S, Goldman IB, Neivert H, et al. Management of deformities of the lower cartilaginous vault. AMA Arch Otolaryngol 1951;54(5):467–472
- Millard DR. Adjuncts in augmentation mentoplasty and corrective rhinoplasty. Plast Reconstr Surg. 1965;36:48–61
- Anderson JR. New approach to rhinoplasty. A five-year reappraisal. Arch Otolaryngol 1971;93(3):284–291
- Peck GC, Jr, et al. An 18-year experience with the umbrella graft on rhinoplasty. Plast Reconstr Surg 1998;102:2158-2165
- Sheen JH. Aesthetic Rhinoplasty. St Louis, MO: Mosby;1978
- Sheen JH. Tip graft: a 20-year retrospective. Plast Reconstr Surg 1993;91:48-63
- Adham MN, Telmourian B. The modified cartilage disc tip graft in primary rhinoplasty. Aesthet Surg J. 1998;18(3):198–201
- Porter JP, Tardy ME Jr, Cheng J. The contoured auricular projection graft for nasal tip projection. Arch Facial Plast Surg. 1999;1(4):312–315
- Guyuron B. Choice of tip augmentation techniques. Op Tech Plast Reconstr Surg 2000;7(4):201-7
- Gruber RP. Nasal tip graft sizing and securing. Op Tech Plast Reconstr Surg 2000;7(4):229-33
- Pastorek NJ, Bustillo A, Murphy MR, Becker DG. The extended columellar strut-tip graft. Arch Facial Plast Surg. 2005;7(3):176–184
- Guyuron B, Jackowe D. Modified tip grafts and tip punch devices. Plast Reconstr Surg. 2007;120(7):2004–2010
- Daniel RK. Tip Refinement Grafts: The Designer Tip. Aesthet Surg J. 2009;29(6):528–537
- Hussein WK, Foda HM. Pollybeak Deformity in Middle Eastern Rhinoplasty: Prevention and Treatment. Facial Plast Surg. 2016;32(4):398–401
- Bussi M, Palonta F, Toma S. Grafting in revision rhinoplasty. Acta Otorhinolaryngol Ital. 2013;33(3):183–189
- Scattolin A, D’Ascanio L. Grafts in “closed” rhinoplasty. Acta Otorhinolaryngol Ital 2013;33:169-176
- Rorich RJ, Deuber MA. Nasal Tip Refinement in Primary Rhinoplasty: The Cephalic Trim Cap Graft. Aesthetic Surg J 2002;22:39-45
